Conditions: hypoglossal nerve injury and dysfunction
What is the hypoglossal nerve?
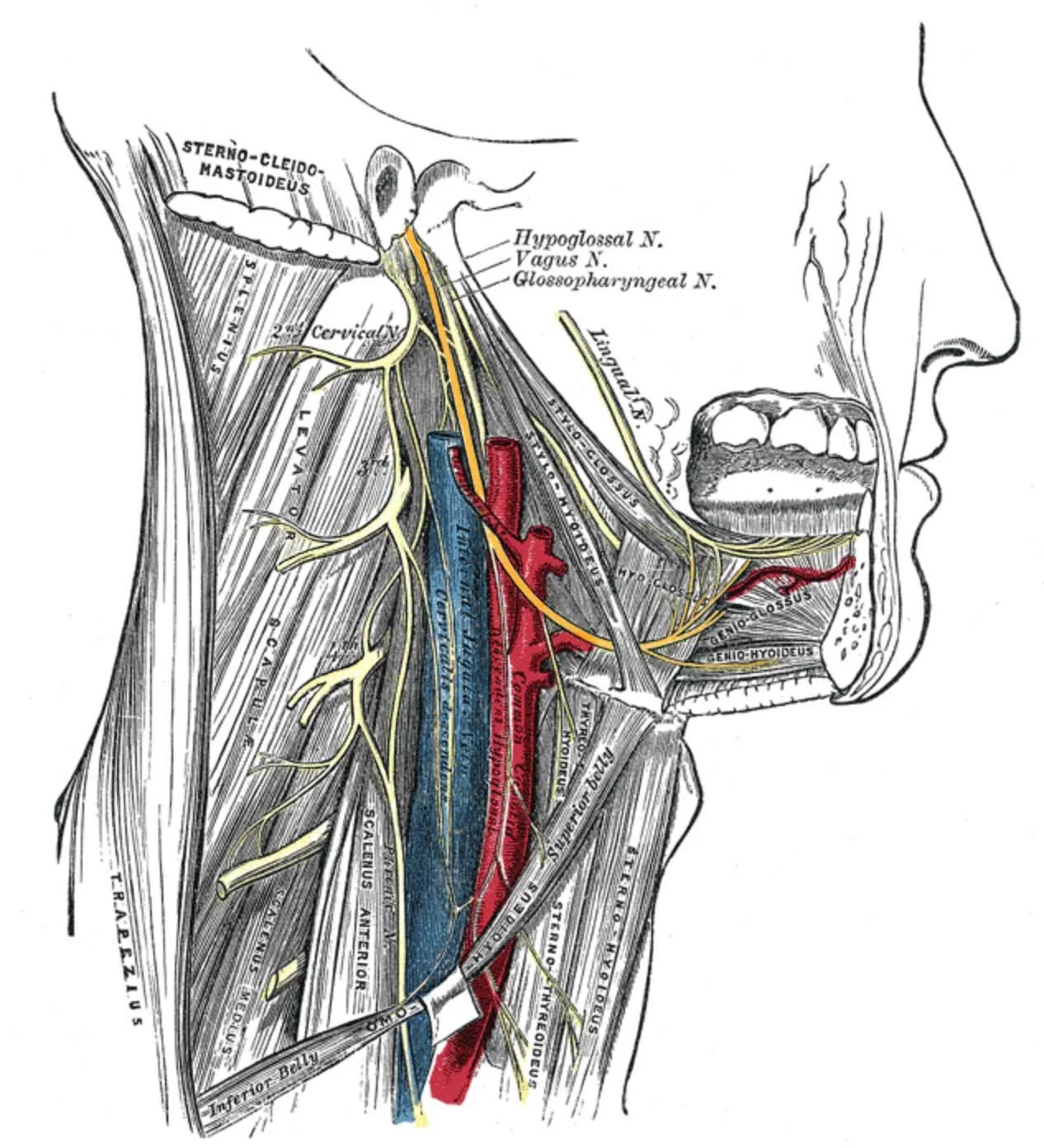
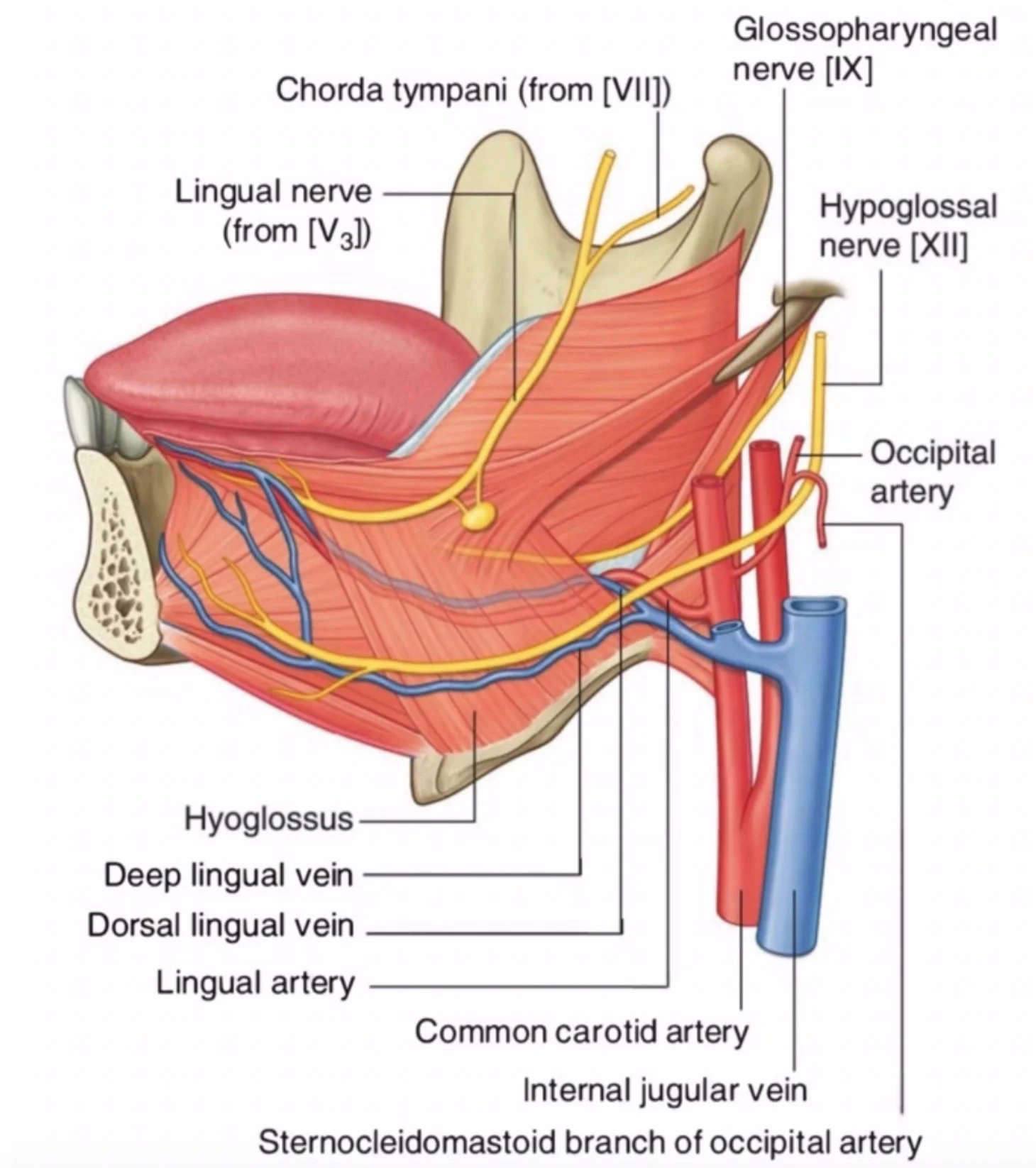
The hypoglossal (twelfth) cranial nerve is responsible for the motor control of the tongue. One left and one right hypoglossal nerve emerges from the brainstem, passes through the skull base into the neck, and courses between the jugular vein and the carotid artery, deep to the submandibular gland, and branches to innervate the target muscles of the tongue on its side.
What causes dysfunction of the hypoglossal nerve?
Various conditions can cause damage and dysfunction of the hypoglossal nerve. Trauma, including gunshot or other penetrating wound and surgery may partially or completely divide the nerve or its branches. Cancer can invade the nerve directly and cause it to become nonfunctional. Stroke, multiple sclerosis, sarcoidosis, Guillain-Barré syndrome, infection, or vascular compression of the nerve can also cause its dysfunction.
Why is the hypoglossal nerve affected by surgery?
Several surgical operations require dissection in proximity to the left or right hypoglossal nerve. Surgery of the upper neck, the submandibular and sublingual glands, tongue, and floor of mouth, for example, involve dissection in proximity of this nerve. Cancer operations may require sacrifice (cutting) of the nerve for the purpose of removing a cancer entirely.
What are the symptoms of hypoglossal nerve weakness?
Dysfunction of the left or right hypoglossal nerve as a whole leads to weakness or flaccidity of that side of the tongue. To a variable degree, this can cause difficulty in enunciating speech as well as manipulating food during the chewing process. Protrusion of the tongue when one nerve is weak is notable for deviation of the tongue toward the weak side. The tongue on the affected side may also loose its firmness and bulk. Over time, an affected individual usually compensates for weakness or paralysis of one side such that speech and food manipulation are minimally impaired.
What precautions are necessary with hypoglossal nerve dysfunction?
The front (anterior) 2/3rd of the tongue is used for speech and manipulation of food during chewing. These functions may be slowed by hypoglossal nerve function and usually respond well to compensation, often with the help of exercises and rehabilitation guided by a speech and language pathologist. The back (posterior) 1/3 of the tongue is used as an important part of swallowing. Impairment of swallowing and possible aspiration (when food or liquid passes into the windpipe/trachea) is a danger when the posterior 1/3 of the tongue functions poorly. Evaluation by a speech and language pathologist and/or obtaining a modified barium swallow study may be indicated to identify and address an impairment in swallowing.
HOw is hypoglossal nerve injury prevented?
While the course of an individual’s nerves, including the hypoglossal nerve is unique, surgeons know the anatomy and make every effort to avoid any injury to the nerve during dissection. Despite all efforts, sometimes hypoglossal nerve weakness or paralysis is unavoidable.
How much will hypoglossal nerve dysfunction bother someone?
Depending on the extent of weakness and if some or all hypoglossal nerve branches are involved with an injury, the degree of bother and impairment is variable. Over time, an affected individual usually compensates for weakness or paralysis of one side such that speech and food manipulation are minimally impaired. Paralysis of both left and right hypoglossal nerves is a significant deficit that may severely compromise speech and the ability to take nutrition by mouth, though rehabilitative efforts may be of benefit.