Conditions: Hyperparathyroidism
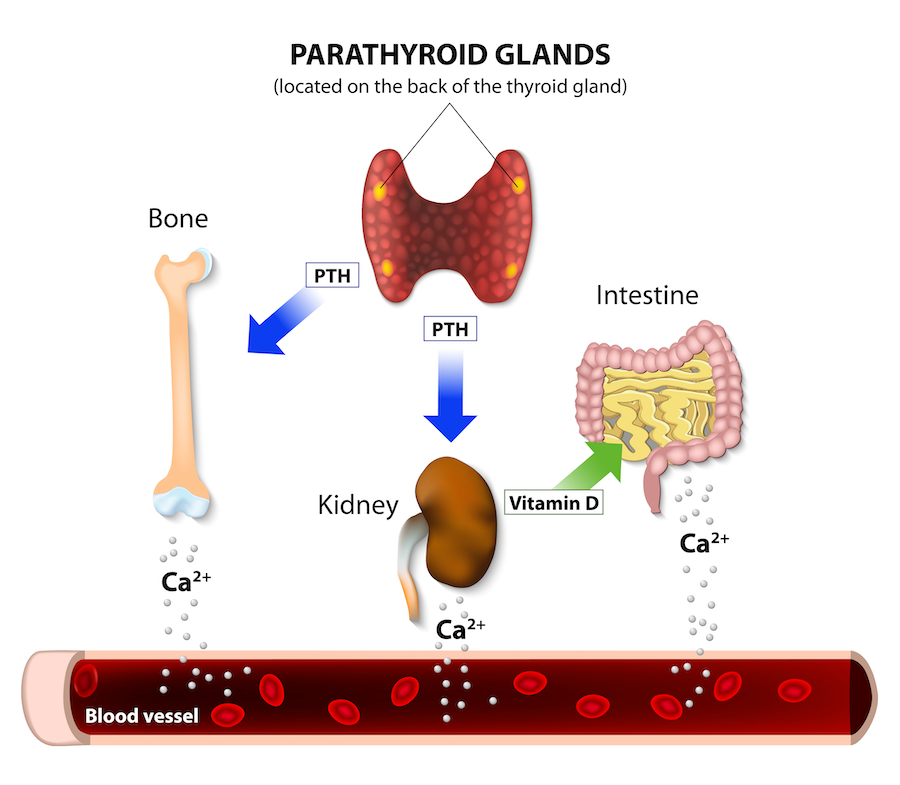
The parathyroid glands are completely different in function from the thyroid gland, but named “parathyroid” because they are located close to the thyroid gland. Parathyroid glands make parathyroid hormone, which circulates in the blood and maintains a concentration of calcium in the blood.
Hyperparathyroidism explained
Parathyroid glands’ job is to detect a low blood calcium level and when this happens, produce parathyroid hormone. This parathyroid hormone is released into the blood and acts on the gut, kidneys, and bones to increase the blood calcium level. When the blood calcium has risen, the parathyroid glands slow or stop the production of parathyroid hormone. This feedback system is the normal mechanism for maintaining a normal calcium level. Unfortunately, parathyroid glands are somewhat prone to getting “stuck in the on position,” or “losing their brakes,” pumping out parathyroid hormone in excess, even when the blood calcium level is high. When this happens, both blood calcium and parathyroid hormone levels are high, a conditioned called primary hyperparathyroidism.
Image edited from Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
This aberrancy is most commonly due to a single parathyroid gland having lost it ability to decrease parathyroid hormone production, but may result from the defect occurring in two, three, or all glands. Genetically, a mutation in the “Menin” gene accounts for the loss of inhibitory function, and the affected gland(s) will grow in size and be called a parathyroid adenoma (a benign parathyroid tumor). In contrast, parathyroid cancer, is a rare condition that causes extremely high parathyroid hormone output and blood calcium levels.
Another form of hyperparathyroidism, called secondary hyperparathyroidism, is characterised by an elevated blood parathyroid hormone, but in contrast to primary hyperparathyroidism, the serum calcium is normal or low. Chronic renal failure and vitamin D deficiency are the most common causes of secondary hyperparathyroidism because both conditions lead to malabsorption of calcium and phosphate, and consequent decreased blood calcium levels that induce normal parathyroid glands to become overactive. In other words, the parathyroid glands are not malfunctioning in secondary hyperparathyroidism—they are responding appropriately to the condition created by kidney disease.
Tertiary hyperparathyroidism is a condition in which the overactive parathyroid glands of secondary hyperparathyroidism fail to revert back to normal parathyroid hormone output despite resolution of the cause of secondary hyperparathyroidism (such as a kidney transplant or correction of vitamin D deficiency).
The opposite of hyperparathyroidism is hypoparathyroidism.
diagnosis of hyperparathyroidism
Most commonly, primary hyperparathyroidism is detected by bloodwork, specifically high blood calcium and parathyroid hormone levels. Once other “look-alike” problems are ruled out, the diagnosis is made. These “look alike” scenarios include use of certain medications (such as lithium) and familial hypocalciuric hypercalcemia. When primary hyperparathyroidism is severe or appears to be causing symptoms, parathyroid surgery is the usual best treatment.
Secondary hyperparathyroidism is also made on the basis of blood tests, but notably is associated with kidney failure (elevated creatinine and BUN), elevated parathyroid hormone, but usually normal calcium levels.
signs and symptoms of hyperparathyroidism
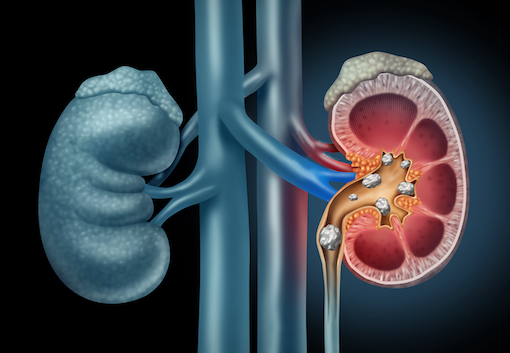
Fatigue, aches and pains, stones (kidney stones, salivary stones), general abdominal aches, and depression are often present to a variable degree with hyperparathyroidism, though the onset may be so slow that the affected individual may not notice the slow change, considering these problems their normal state of being or age. The symptoms of hyperparathyroidism are non-specific. For example, fatigue is a common symptom of hyperparathyroidism, but not everyone with fatigue has hyperparathyroidism. This lack of clear association between hyperparathyroidism and symptoms is why the diagnosis of hyperparathyroidism is often first made by bloodwork. Hyperparathyroidism also slowly removes calcium from bones, leading to osteopenia or osteoporosis, which reduces bone strength and increasing risk of bone fracture.
sestamibi parathyroid scan
Since we typically have four parathyroid glands, and since their location may be different in different individuals, a scan to locate the one or more parathyroid glands that are working too much is commonly done prior to surgery so that the operation can be quicker and more anatomically focused. It is important to note that an imaging study is not useful in making a diagnosis of hyperparathyroidism, but rather, only trying to identify the site of one or more overactive glands (parathyroid adenomas) after the diagnosis has been made.
For finding enlarged parathyroid glands, the technique entails delivery of the gamma-emitting radioisotope technetium-99m into the patient, by injecting it into the bloodstream. The technetium-99m collects in certain types of tissues, including parathyroid glands, salivary glands, and the heart. The scanned image is often conclusive and accurate, but occasionally the study fails to reveal a clear-cut parathyroid adenoma, which may be due to the enlargement of multiple parathyroid glands or the failure of one or more parathyroid adenomas to take up the technetium-99m.
SPECT (Single positron emission ct) scan
Single-photon emission computed tomography (SPECT) is a nuclear medicine tomographic imaging technique using gamma rays. It is very similar to conventional nuclear medicine imaging but is able to provide true 3D information. This information is typically presented as cross-sectional slices through the patient, but can be freely reformatted or manipulated as required. It is often combined with a imaging CT scan, and the hybrid of both image types for improved anatomic accuracy.
symptoms of low parathyroid hormone and low calcium
Low parathyroid hormone (hypoparathyroidism) and consequent low calcium is sometimes present after neck surgery if the procedure caused the parathyroid glands to decrease production of parathyroid hormone. When it happens, it may be only temporary, as parathyroid glands may be stunned for a week or so just from manipulation. A mild decrease in blood calcium may be inconsequential, but avoiding severely low calcium levels is important. Symptoms of low calcium levels can include numbness or tingling, especially on the fingertips or the lips, and muscle spasms (like a “Charlie horse”). Notify your doctor if you experience either of these symptoms after neck surgery. A blood draw may be used to objectively determine the blood calcium level.
Get the most from your parathyroid appointment
Appointment time is valuable. Below are some suggestions to make the most of your appointment. This preparation will help you and your doctor maximize efficiency and accuracy, freeing up time for questions and answers.
This page