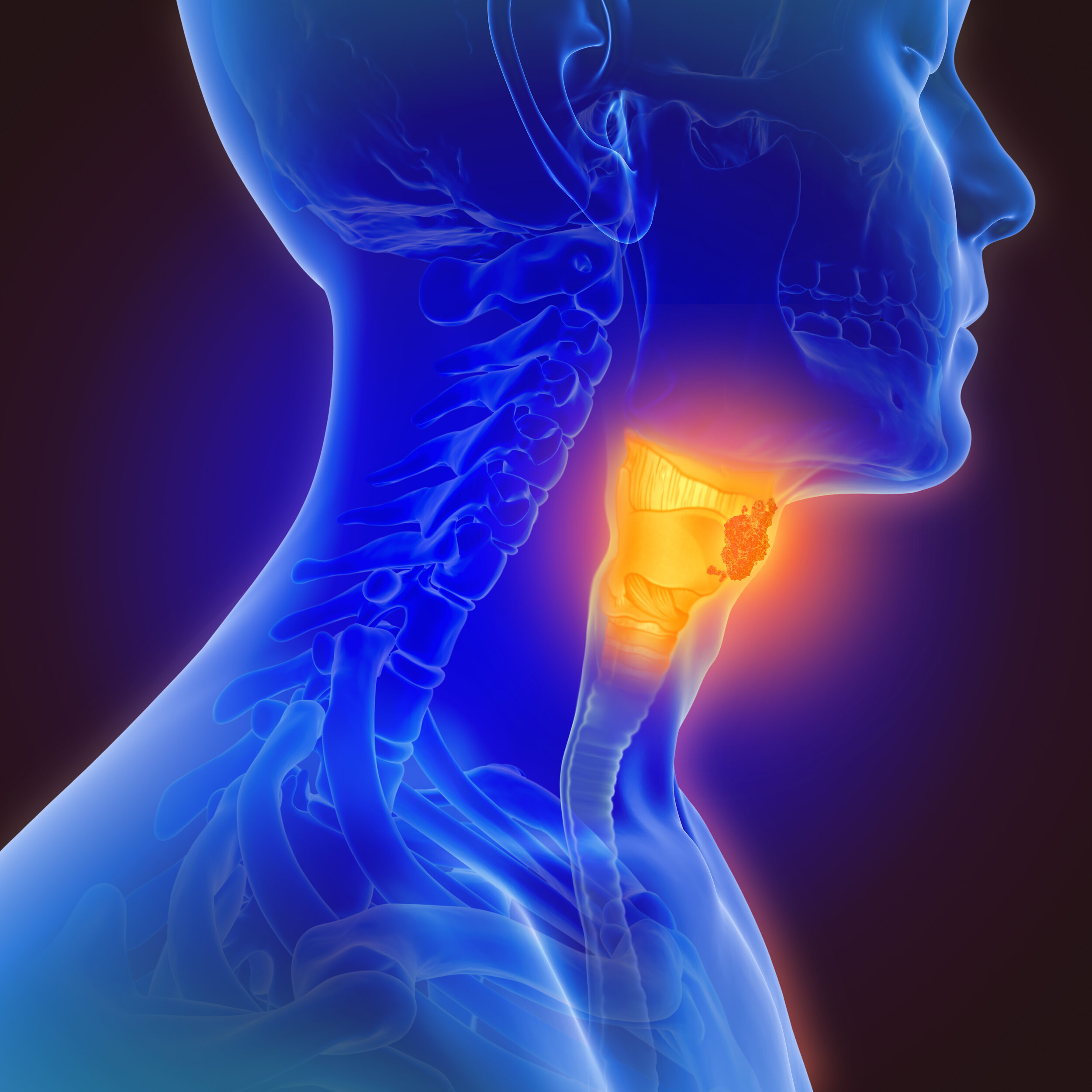
Treatments: Throat Tumors
Treating throat cancer involves choosing the best treatment type (surgery, radiation, medical, or a combination), getting through treatment, and playing an active role to retain the best long-term function possible. The specific anatomic location and the type of cancer are major factors in determining treatment options.
Anatomic sites for throat cancer
Nasopharynx - the site of nasopharyngeal carcinoma
Oropharynx - the site of oropharyngeal (including base of tongue and tonsil) tumors, commonly squamous cell carcinoma,
Hypopharynx - the site of pyriform sinus tumors, commonly squamous cell carcinoma
Carcinoma from each of these sites may spread to lymph nodes of the neck (called regional spread), or to more distant sites such as the lungs.
cancer treatment: The tools in the toolbox and which are chosen
Broadly speaking there are three main ways to treat cancer: surgery, radiation, and medicine. These are often used in combination and which tools are used, the sequence in which they are used, and many other facets of exactly how a treatment plan develops is the product of much thought. Tumor board is a group of experts from various different specialties (surgical oncology, medical oncology, radiation oncology, radiology, pathology, nursing, social work, dietary, and others) that get together to review the current cancer cases. After reviewing the history and exam findings, the imaging studies and pathology, discussion ensues in which the current best evidence-based practice is applied to an individual situation whereby a consensus recommendation by the tumor board group is rendered. This is presented to the patient who ultimately decides how he or she wishes to proceed.
radiation therapy
Radiation therapy is generally effective and one of the standard treatment options for cancers of the throat and surrounding areas where a cancer may have spread (such as the lymph nodes of the neck). It works like a very fancy flashlight, except instead of shooting photons of light at a target, it shoots electrons. Modern radiation machines have the ability to shoot the electrons from many different angles so that the cancer accumulates the optimal dose and the normal structures around the target (such as the spinal cord or the eyes, for example) get a minimal dose. There is absolutely no radioactivity left in the patient after treatment—it’s not that kind of radiation. A custom mask is made to position you in exactly the same position for every treatment, and once the planning is complete, treatments lasting only about ten minutes each can begin. Treatments are usually once a day (but sometimes two). Monday through Friday, and usually last about six weeks. The first two weeks usually go by without side effects, and then a sore throat, a sunburned reaction on the skin, and some fatigue set in. This progresses until about two weeks after the radiation is complete and then begins to resolve. The body is just now beginning to ramp up the scar tissue formation, and movement is the only way to prevent fixation of the neck and throat muscles into immobile and poorly functioning tissue! Swallowing and range of motion exercises of the jaw and neck throughout and after radiation therapy are essential to prevent irreversible fixation of the neck and throat. Physical therapy and swallowing exercises are highly beneficial in this regard. Scar formation peaks at about 2-4 weeks from the treatment, but continuous collagen (scar) production and degradation has the effect of remodeling the wound for approximately six months, so one must continue diligent efforts for several months after treatment.
medical therapy (chemotherapy and immunotherapy)
Medical therapy for cancer is usually administered by a medical oncologist. Several different types of throat cancer exist, but squamous cell carcinoma is by far the most common type of cancer of the throat, and for this type of cancer, chemotherapy is sometimes given during (in addition to) radiation therapy to make the radiation more effective. When used together, radiation is usually given five days a week (Monday through Friday) and chemotherapy is also given one day a week. Using both chemotherapy and radiation simultaneously is more effective against squamous cell carcinoma, but it also has more side effects. This is the reason combination therapy is recommended only when there is high risk of treatment failure with radiation alone. The usual chemotherapy drug used is either cis-platin or carboplatin, similar chemically and based on platinum in the molecule. Side effects of these platinum-based chemotherapies include nausea, low blood counts, decreased kidney function, and hearing loss and ear ringing (tinnitus). Immunotherapy, on the other hand, is a strategy in which drugs tap into the power of the immune system to kill cancer cells. Immunotherapy is often used after other treatments (such as surgyer, radiation, and/or chemotherapy) are complete and may be continued over extended periods of time. (Another type of cancer frequently present in the neck is lymphoma, which is treated with different medicines as the main weapon and radiation is used much less commonly).
surgery through the mouth (including robotic surgery)
Surgery is also a widely accepted and effective treatment method for throat cancer. Surgical treatment is best applied when it has a high chance of removing the cancer entirely and when healing time, operative risks, and any functional losses after surgery are minimal compared to other treatment options. The surgical approach to throat cancer is typically through the mouth, and neck surgery (through a skin incision) for removal of the lymph nodes is often performed simultaneously. Tissue borrowed from another part of the body may be used to assist in reconstruction of the throat. A hospital stay is common, with discharge possible when it is deemed safe.
Removal of lymph nodes (cervical lymphadenectomy or “neck dissection”)
Throat cancers tend to be the type of cancer with a predisposition to spread to lymph nodes of the neck. If one or more lymph nodes appears to have cancer spread to it or if there is high risk for spread to the lymph nodes, any surgical approach to the primary tumor (where the cancer started) is often combined during the same operation with removal of those lymph nodes. This procedure, when done is skilled and experienced hands, can remove cancerous lymph nodes with maximal preservation of the important nerves, muscles, and blood vessels in the neck.
voice box (larynx) surgery
Always with cure and preservation of function at the forefront of thought, surgery is utilized sometimes instead of, or in conjunction with radiation therapy or medical therapy for larynx cancers. In select cases, surgery performed through the mouth using a robot or an endoscope can remove a cancer above the vocal cords (supraglottic laryngectomy). If one or both vocal cords are involved with cancer, then techniques involving the removal some or all of the voice box (partial laryngectomy, total laryngectomy, respectively) may be undertaken. Removal of the lymphatic tissue (cervical lymphadenectomy) is usually combined with these procedures due to known or potential spread of cancer to the nearby lymph nodes. Tissue from another part of the body is sometimes borrowed to facilitate reconstruction of the throat after cancer removal. Risks, benefits, and expected outcomes of surgery are compared to those from other options, such as radiation or radiation plus chemotherapy for each individual.
how to maintain swallow function after treatment
The value of functional, safe swallowing cannot be overemphasized, but swallowing is at risk with throat cancers and their treatment. The best swallow results come through an active and effortful role on the part of the patient, guided with a speech and language pathologist (swallowing specialist).
How to maintain neck, jaw, and shoulder range of motion and strength after treatment
Jaw opening, neck flexibility, and shoulder strength (specifically, raising your arm above your head as in a jumping jack) are tremendously important for daily activity, but are at risk after treatment of head and neck cancer. Maintaining function is possible, but only through an effortful and active process of exercises. Physical therapy involving treatment of lymphedema, range of motion and strengthening (including jaw opening work by a speech and language pathologist) is often the foundation for success, but diligently performing the exercises is the key ingredient.
This page