Conditions: Hypoparathyroidism
What is hypoparathyroidism?
Hypoparathyroidism is an endocrine disorder characterized by insufficient production of parathyroid hormone (PTH) by the parathyroid glands. These small glands, usually four in number and usually located adjacent to the thyroid gland in the neck, play a major role in regulating calcium and phosphorus levels in the blood. With low or absent PTH levels, low calcium levels (hypocalcemia) and high phosphorus levels (hyperphosphatemia) occur. Of note, while hypoparathyroidism causes hypocalcemia, but hypocalcemia may be caused by several other conditions besides hypoparathyroidism.
How do the parathyroid glands normally function?
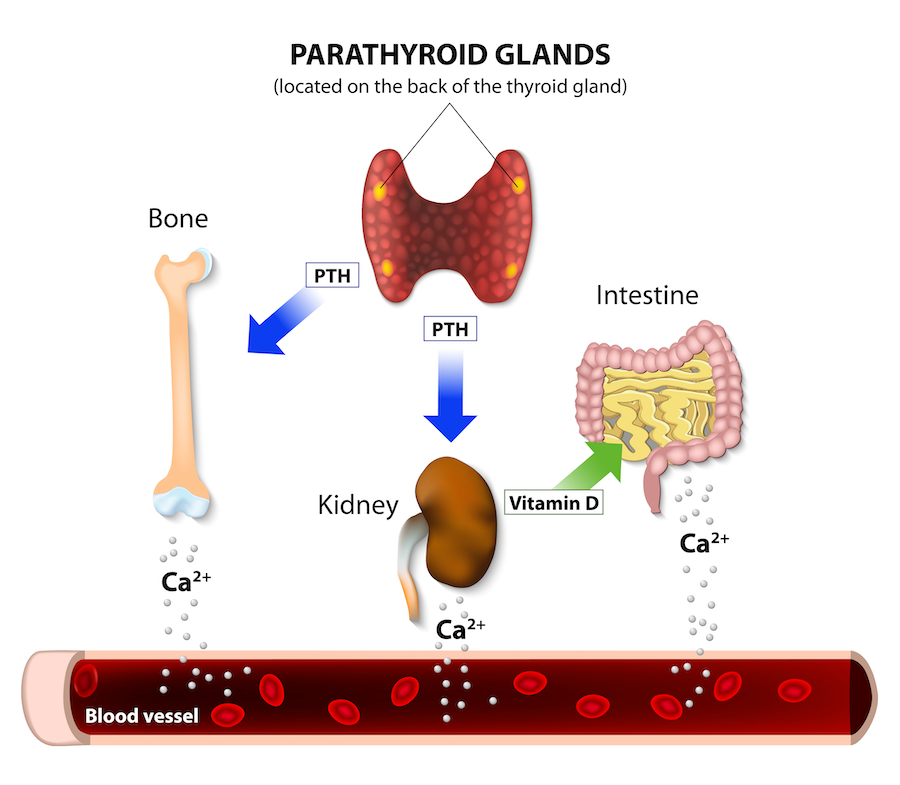
The parathyroid glands play a crucial role in maintaining calcium levels in the body. These small, pea-sized glands, located in the visceral space of the neck (near the thyroid gland), produce and release parathyroid hormone (PTH). Normally, the parathyroid glands function by constantly monitoring the blood calcium levels. When the calcium levels drop, the parathyroid glands release PTH into the bloodstream. PTH stimulates the bones to release calcium into the blood, promotes calcium reabsorption by the kidneys, and enhances the absorption of calcium from the intestines. This concerted action of the parathyroid glands ensures that there is a sufficient supply of calcium in the blood to support proper nerve function, muscle contraction, blood clotting, and bone health. Conversely, when blood calcium levels are high, the parathyroid glands reduce the production and release of PTH, which helps prevent the excessive build-up of calcium in the blood.
what causes hypoparathyroidism?
Loss or dysfunction of all parathyroid glands is necessary to result in hypoparathyroidism. Although most individuals have four parathyroid glands, as little as one half of one gland can produce enough parathyroid hormone to regulate calcium normally. This redundancy is advantageous because surgery near the parathyroid glands (including surgery of the thyroid, parathyroid, nearby lymph nodes, upper trachea and upper esophagus) does risk unintended injury to or removal of one or more parathyroid glands. As the parathyroid glands are normally very small, are located in variable anatomic positions, can look like the surrounding tissues (thyroid, lymph node, or fat), have a very small blood supply, unintended loss of one or more parathyroid glands during nearby surgery may occur despite every effort to preserve them.
Despite the variable number and location of parathyroid glands, it is extremely uncommon for an individual not to have at least one left and at least one right gland at birth. And since as little as one half of one parathyroid gland is sufficient for normal parathyroid function, surgery on only one side of the visceral space of the neck has an essentially nonexistent risk of causing hypoparathyroidism. Surgery on both sides of the visceral space of the neck, whether in one operation or cumulatively over time, does incur risk of hypoparathyroidism.
Non-surgical causes of hypoparathyroidism are much less common, but include an autoimmune condition (autoimmune polyendocrine syndrome), rare genetic defects, magnesium deficiency, or radiation therapy to the visceral space of the neck.
what are the effects of hypoparathyroidism?
Untreated hypoparathyroidism results in low levels of calcium in the blood (hypocalcemia), which may cause symptoms such as muscle cramps, tingling or numbness in the fingers and toes, fatigue, and in severe cases, muscle spasm (tetany), hear rhythm problems, and seizures.
Additionally, long-term effects of hypoparathyroidism may include:
Neurological complications: Prolonged hypocalcemia can cause cognitive disturbances, such as memory problems or anxiety, and in severe cases, seizures.
Skeletal changes: Abnormal calcium and phosphate balance can affect bone metabolism, leading to accrual of bone (increased bone density) without normal bone remodeling. Whether this unremodeled bone is weaker than normal bone is not currently clear.
Dental problems: Defects in tooth enamel formation and root abnormalities.
Calcifications: Ectopic calcifications may occur in the basal ganglia or other brain regions, which can impact neurological function.
Weakness, fatigue, cataracts, brittle nails, dry scaly skin may also be promoted by chronic hypoparathyroidism.
Is hypoparathyroidism temporary or permanent?
It depends. Hypoparathyroidism after surgery is temporary about 75% of the time. If hypoparathyroidism persists for longer than about one month after surgery, then it is likely to be permanent. Early prediction of whether post-operative hypoparathyroidism will resolve is not always possible, but several factors may help inform the situation while waiting for return of parathyroid function. One major clue is the assessment of the surgeon. If one or more parathyroid glands were seen at the time of surgery to be preserved and with a good vascular supply, this strongly favors resolution of any post-operative hypoparathyroidism. A blood draw showing any detectable parathyroid hormone after surgery is also a strong indicator that parathyroid function will normalize. A slow decline in calcium levels after surgery is also more predictive of a temporary hypoparathyroidism than with a steep decline in calcium levels.
Specific scenarios of hypoparathyroidism include:
After parathyroid surgery, when one or more overactive parathyroid glands are removed, the remaining parathyroid glands need time to become fully active. As with muscles, unused parathyroids atrophy over time. When one parathyroid is over-active, thus raising the calcium level in the blood, the other parathyroid glands appropriately reduce their own production of parathyroid hormone. Once surgery is undertaken and the overactive gland has been removed, the other glands need some time to build up and produce the needed amount of parathyroid hormone.
After surgery of or around the parathyroid glands, including parathyroidectomy, total or completion thyroidectomy, and laryngectomy, parathyroid glands that are manipulated during the operation may be “stunned”—that is, rendered temporarily inactive. Return of normal parathyroid function in this scenario may take a week or two.
If all parathyroid glands are removed or die due to lack of blood supply, then the resultant hypoparathyroidism may be permanent.
how is hypoparathyroidism treated?
The mainstay treatment of hypoparathyroidism is supplementation with calcium and/or vitamin D. For new hypoparathyroidism after surgery, calcium replacement or vitamin D can improve the low calcium and the associated symptoms. Checking blood magnesium and supplementing any deficiency helps the kidney retain calcium. Mild hypocalcemia may be treated with oral calcium. As the severity of hypocalcemia worsens, increasing doses given more frequently may be used. For additional boost in serum calcium, oral vitamin D may be given, also with dose and frequency according to need. More severe hypocalcemia may be treated with intravenous calcium gluconate, which typically requires being in a healthcare facility.
Repeated blood draws are used to assess the blood concentration of calcium, and possibly also albumin (to accurately interpret blood calcium levels), parathyroid hormone level, and magnesium. When parathyroid function shows improvement over time, the regimen of medications for treating low calcium may be gradually lessened as the calcium level improves.
In the case of hypoparathyroidism that does not improve in the month or two, which indicates permanence of hypoparathyroidism, treatment will include long-term vitamin D and calcium supplementation. Periodic monitoring of blood calcium is necessary, and the target calcium levels are at the lower limit of normal to miminize risk of kidney problems such as kidney stones and worsened kidney function. Kidney ultrasound examinations may also help in monitoring for associated kidney problems.
A newer strategy for treatment of permanent hypoparathyroidism is use of a parathyroid hormone analog medication. Palopegteriparatide (Yorvipath®) is the current parathyroid hormone analog administered as a daily, subcutaneous (under the skin) injection using a prefilled, disposable pen.
The disadvantages of parathyroid hormone replacement include that the medication is not available in oral form, and that use may increase risk of a bone cancer called osteosarcoma. Increased rates of osteosarcoma were observed in rats treated with PTH analogs like palopegteriparatide, and the risk was dependent on the dose and duration of treatment. While observational studies in humans using other PTH analogs have not shown an increased risk compared to the general population, data on longer-term use is limited. The U.S. Food and Drug Administration (FDA) and other health authorities include this risk in the drug's labeling to inform both prescribers and patients.
Long term management of hypoparathyroidism is usually undertaken under the care of an endocrinologist.