Oropharyngeal Squamous Cell Carcinoma
The oropharynx is the middle part of the throat, including the base of the tongue and the tonsils. Squamous cell carcinoma is by far the most common type of cancer in the oropharynx. An important difference between the two major subtypes of oropharyngeal squamous cell carcinoma are those that are caused by the Human Papilloma Virus (HPV) and those that are not.
What is Oropharyngeal Squamous Cell Carcinoma (OPSCC)
Oropharyngeal squamous cell carcinoma (OPSCC) is a type of cancer that arises from the cells lining the oropharynx, which includes the base of the tongue, tonsils, and soft palate.
What causes oropharyngeal squamous cell carcinoma of the oropharynx?
Fundamentally, for a normal cell to become a cancer, one or more genetic mutations in a cell’s DNA occurs leading to a set of changes promoting cell growth, division, and aggressive behavior. There are two categories of causes of the genetic mutations leading to OPSCC:
Human papilloma virus (HPV): Certain strains of the human papilloma virus, particularly HPV types 16 and 18, can cause oropharyngeal squamous cell carcinoma. Transmission typically occurs through contact with this virus (most commonly by oral sex).
Non-HPV conditions: OPSCC can also be caused by exposure to tobacco, especially associated with heavy alcohol consumption, and poor oral hygiene. Other risk factors may include age, gender (more common in males), and certain dietary factors. Rarely, either due to a genetic predisposition or reasons unknown, a person without exposure to known risk factors can develop squamous cell carcinoma.
Attribution of the Cause in a Given Individual
Determining the cause of OPSCC is useful because HPV driven OPSCC behaves differently and responds to treatment better than HPV negative OPSCC. The presence of protein called p16 corresponds very highly with the presence of HPV in OPSCC. Since testing for p16 is much simpler and faster than is testing for HPV directly, p16 is used as a surrogate marker for HPV in this setting. For the most part, with reasonable accuracy, a given individual’s cause for OPSCC may be put in one of these categories:
Human papilloma virus (HPV) caused OPSCC: Tumors caused by HPV have HPV DNA within them and produce certain proteins, most prominently p16 at high levels. Identifying high amounts of p16 in a specimen of OPSCC (called p16 positive) is usually used to deduce the presence of HPV in the tumor.
Non-HPV caused OPSCC: Low or absent amounts of p16 in a specimen of OPSCC (a situation called HPV negative) is interpreted to mean the cancer was not caused by HPV. Patients in this category usually have known risk factors for OPSCC other than HPV, such as a significant tobacco use history with or without high alcohol consumption and poor oral hygiene.
Indeterminant caused OPSCC: In some cases, a patient may have a significant history of tobacco use but the tumor biopsy may also be p16 positive. In this case, either or both risk factors could have caused the cancer. For practical purposes, data shows that when a tumor is p16 positive and a patient has smoked less than 10 pack years of cigarettes (the equivalent number of cigarettes in smoking one pack per day for 10 years), the tumor behaves more like HPV positive (p16 positive) OPSCC. When the tumor is p16 positive and the patient has smoked more than 10 pack years of cigarettes, the tumor behaves somewhat more like OPSCC not caused by HPV.
Diagnosis
Diagnosis of OPSCC often involves several steps:
Medical History and Physical Examination: Healthcare providers will assess symptoms such as sore throat, difficulty swallowing, changes in voice, or the presence of lymphadenopathy (swelling of lymph nodes).
Imaging Tests: Imaging techniques such as CT scans, MRI, or PET-CT scans may be utilized to evaluate the extent of the disease and identify any metastasis.
Biopsy: A definitive diagnosis is made through a biopsy of the suspicious lesion, where tissue samples are examined histologically for the presence of cancerous cells. Depending on the situation, biopsy may be undertaken by removing a small piece of the throat tumor either in the office or in the operating room, or by performing a needle biopsy of a neck mass. The biopsy specimen may be tested for p16 or, less commonly, with other techniques for identification of HPV.
Treatment
In a very general sense, there are three main modes of treatment for cancer: surgery, radiation, and medicine. This is true for OPSCC.
Surgery may be used to remove the primary tumor (the original site of development, in the oropharynx), regions of involved or at-risk lymph nodes in the neck, and/or sometimes distant spread to other parts of the body (such as the lung or lymph nodes in the chest).
As with surgery, radiation may be used to treat an anatomic region, such as the site of the primary tumor, the involved or at-risk lymph nodes in the neck, and/or somemtimes distant spread to other parts of the body.
Medicine to treat OPSCC includes both chemotherapy and immunotherapy. Chemotherapy is medicine given IV that is toxic to cancer cells more than non-cancerous cells. Immunotherapy is medicine that uses the body's own immune system to fight the cancer by enhancing or restoring its ability to recognize and attack the cancer cells.
One, two, or all three of these treatment modalities may be used for a given cancer. A treatment plan recommendation for a given individual is based on the specifics of their cancer—this includes the stage, presence of adverse features (such as growth along nerves or blood vessels, or a lymph node with cancer that ruptures beyond the capsule of the lymph node) and general health considerations. OPSCC is at an early stage (limited size and limited spread), one or two modalities may be used, such as surgery alone, radiation alone, or surgery plus radiation. More advanced cancers are typically treated with more modalities of treatment, including all three (triple therapy of surgery followed by chemotherapy and radiation therapy), but with greater cancer kill of multiple modalities also comes greater side effects.
ANATOMY
The throat (pharynx) is anatomically divided into three parts: the nasopharynx at the back of the nose, the oropharynx behind the oral cavity, and the hypo pharynx just above the esophagus. The larynx (voice box) is in front of the hypopharynx and is the entryway into the trachea.
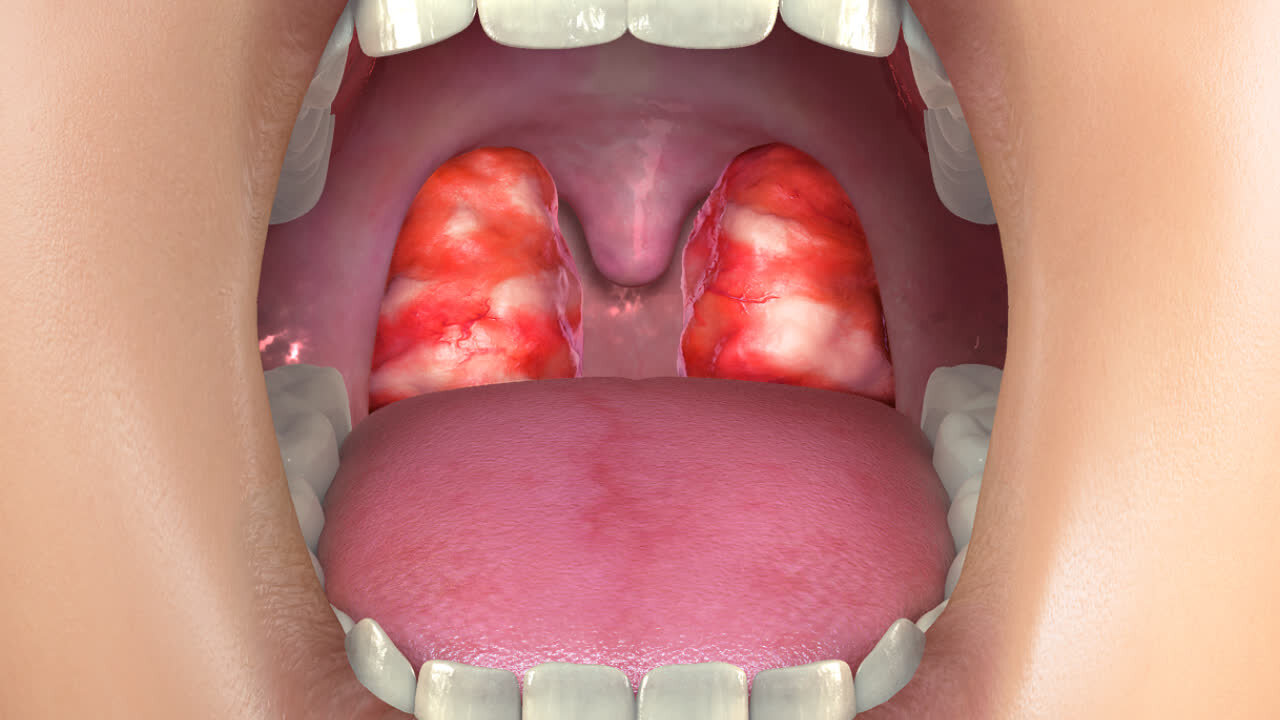
The oropharynx includes the tonsils and the base of tongue, both of which contain lymphatic tissue that HPV tends to infect preferentially. For this reason, HPV caused OPSCC is typically in a tonsil or the base of tongue. OPSCC not caused by HPV can also occur in a tonsil or the base of tongue, but is more likely than HPV caused cancer to also occur in the soft palate or the back of the throat, where there is minimal lymphatic tissue.
Tonsil cancer
Tonsils (technically, the “palatine tonsils”) are lumps of tissue in the sides of the oropharynx. While tonsils may become swollen and/or infected, certain characteristics of an enlarged tonsil raise suspicion for possible cancer. These include a history of smoking with or without heavy drinking, the presence of one or more lumps in the neck, one tonsil being significantly larger than the other, and bleeding from a tonsil. The three most common types of tonsil cancer are p16 positive squamous cell carcinoma, p16 negative squamous cell carcinoma, and lymphoma.
base of tongue cancer
The very back of the tongue, which is not visible when looking directly through an open mouth, is called the base of the tongue, and its surface has a layer of tissue identical to the tonsil. In fact, this tissue is often called "lingual tonsil” meaning tonsil of the tongue. The base of the tongue is a specific site within the broader anatomic area called the oropharynx. As with palatine tonsils, the lingual tonsils can develop into cancers of various types described above (p16 positive squamous cell carcinoma, p16 negative squamous cell carcinoma, and lymphoma, among others). A growth in this location is can grow surprisingly large before it is noticed, and often the first indication of a problem is the development of a lump in the neck due to spread of the cancer to a lymph node.
Functions that may be affected by oropharynx cancer and it treatment:
Swallowing
Swallowing well is essential for maintaining nutrition as well as avoiding aspiration (when food or liquid passes into the lungs), which can lead to severe pneumonia. Cancers of the oropharynx may lead to problems swallowing, not only because of the tumor size, but also because treatments may affect the ability to swallow comfortably, effectively and safely. A speech and language pathologist is helpful in the evaluation and mitigation of swallowing deficits associated with OPSCC. When the swallowing difficulty is severe, one may need to consider placement of a gastric feeding tube (G tube).
Hearing
The mass of an OPSCC may directly block the entrance to the Eustachian tube, causing Eustachian tube dysfunction. Treatment for the cancer, especially radiation therapy with or without chemotherapy, can also create long-term Eustachian tube dysfunction. The most commonly used chemotherapy medications used for OPSCC, cisplatin and carboplatin, have the unfortunate consequence of often damaging the cochlea (inner ear hearing organ), resulting in sensorineural hearing loss. Repeated evaluations by a head and neck surgeon and an audiologist are therefore necessary from the time of the cancer diagnosis onward.
Breathing
Large mass OPSCC may block the airway. The tumor mass generally grows slowly, but breathing difficulty may uncommonly progress from mild airway restriction to a respiratory crisis. In this uncommon situation of an airway threatened by the bulk of an OPSCC, surgical placement of a tracheostomy tube may be necessary as a life-saving measure. Also very uncommonly but depending on the specific situation, a person may. require a tracheostomy tube temporarily or permanently after OPSCC treatment is complete.
speech
As the oropharynx is part of the mechanism for speaking, both a tumor itself and the tissue changes associated with treatment may affect one’s ability to speak easily and effectively. Consultation and therapy with a speech and language pathologist is often very helpful in maximizing speech ability after therapy for OPSCC.
Get the most from your throat tumor appointment
Appointment time is valuable. Below are some suggestions to make the most of your appointment. This preparation will help you and your doctor maximize efficiency and accuracy, freeing up time for questions and answers.
This page